Interlaminar Endoscopic Spine Surgery
- Home >>
- Interlaminar Endoscopic Spine Surgery
What is Interlaminar Endoscopic Spine Surgery?
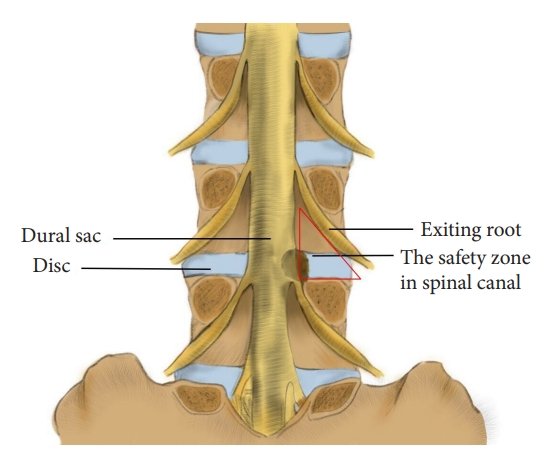
Interlaminar endoscopic spine surgery is a minimally invasive procedure that uses a small endoscope (a thin tube with a camera and light) inserted through the interlaminar window to treat spinal pathologies. The interlaminar approach targets the posterior spine, accessing structures like the spinal canal, nerve roots, or discs without extensive muscle dissection. It is commonly used for lumbar and thoracic spine conditions but can be adapted for specific cases, such as spinal TB-related complications (e.g., abscesses, disc damage, or nerve compression).
In the context of spinal TB, this technique may be employed to debride infected tissue, relieve nerve compression, or address deformities while minimizing surgical trauma, complementing anti-TB therapy and other interventions like those in interventional pain management.
Types of Interlaminar Endoscopic Spine Surgery
Interlaminar endoscopic spine surgery encompasses several techniques, depending on the pathology and spinal region. Key types include:
- Interlaminar Endoscopic Discectomy:
- Description: Removes herniated disc material compressing nerves or the spinal cord via the interlaminar window.
- Uses: Lumbar disc herniation, sciatica, or disc damage from TB-related infection.
- Spinal TB Relevance: Addresses disc destruction or nerve compression caused by TB.
- Interlaminar Endoscopic Decompression:
- Description: Relieves pressure on the spinal cord or nerves by removing bone (lamina), ligaments, or scar tissue.
- Uses: Spinal stenosis, foraminal stenosis, or TB-related epidural abscesses causing compression.
- Spinal TB Relevance: Clears abscesses or scar tissue impacting neurological function.
- Interlaminar Endoscopic Foraminotomy:
- Description: Enlarges the neural foramen (nerve exit) to relieve nerve root compression.
- Uses: Foraminal stenosis or nerve impingement from TB-related vertebral collapse.
- Interlaminar Endoscopic Debridement:
- Description: Removes infected or necrotic tissue using endoscopic tools.
- Uses: Spinal TB abscesses, osteomyelitis, or localized infection.
- Spinal TB Relevance: Directly targets TB-infected tissue, reducing bacterial load.
- Interlaminar Endoscopic Fusion (Emerging):
- Description: Stabilizes the spine by placing grafts or implants endoscopically, though less common.
- Uses: Instability from TB-related vertebral destruction or post-debridement stabilization.
Benefits of Interlaminar Endoscopic Spine Surgery
This technique offers significant advantages, especially for spinal TB patients requiring surgical intervention:
- Minimally Invasive:
- Small incisions (5–10 mm) reduce muscle and tissue damage compared to open surgery, leading to less postoperative pain and scarring.
- Spinal TB Example: Minimizes trauma in already compromised tissues due to infection.
- Faster Recovery:
- Patients often resume activities within days to weeks, compared to months for open surgery.
- Spinal TB Example: Allows quicker return to physiotherapy, crucial for TB recovery.
- Reduced Blood Loss:
- Precise endoscopic tools minimize bleeding, lowering transfusion risks.
- Spinal TB Example: Beneficial for patients with systemic TB symptoms like anemia.
- Lower Infection Risk:
- Smaller incisions and shorter hospital stays reduce postoperative infection rates, critical for TB patients with compromised immunity.
- High Precision:
- Endoscopic visualization provides magnified views of spinal structures, enabling accurate targeting of pathology.
- Spinal TB Example: Ensures thorough debridement of infected tissue while sparing healthy structures.
Procedure for Interlaminar Endoscopic Spine Surgery
The process for interlaminar endoscopic spine surgery follows a standardized protocol, with adaptations based on the specific condition (e.g., spinal TB). Here’s a step-by-step overview:
- Preoperative Evaluation:
- A spine specialist (e.g., Dr. Nevish Patel or Dr. Ankit Khodifad) reviews the patient’s history, symptoms, and imaging (MRI/CT) to confirm pathology (e.g., TB-related abscess or disc herniation).
- Neurological exams assess deficits like weakness or numbness.
- For spinal TB, microbiological confirmation (e.g., biopsy) may precede surgery to guide anti-TB therapy.
- Procedure Planning:
- The surgeon selects the interlaminar approach based on the lesion’s location (e.g., lumbar or thoracic spine).
- Risks (e.g., nerve injury, infection) and benefits are discussed with the patient.
- Preparation:
- Performed under general or local anesthesia with sedation, depending on the case.
- The patient is positioned prone (face-down) on a specialized table.
- Fluoroscopy or intraoperative imaging ensures precise endoscope placement.
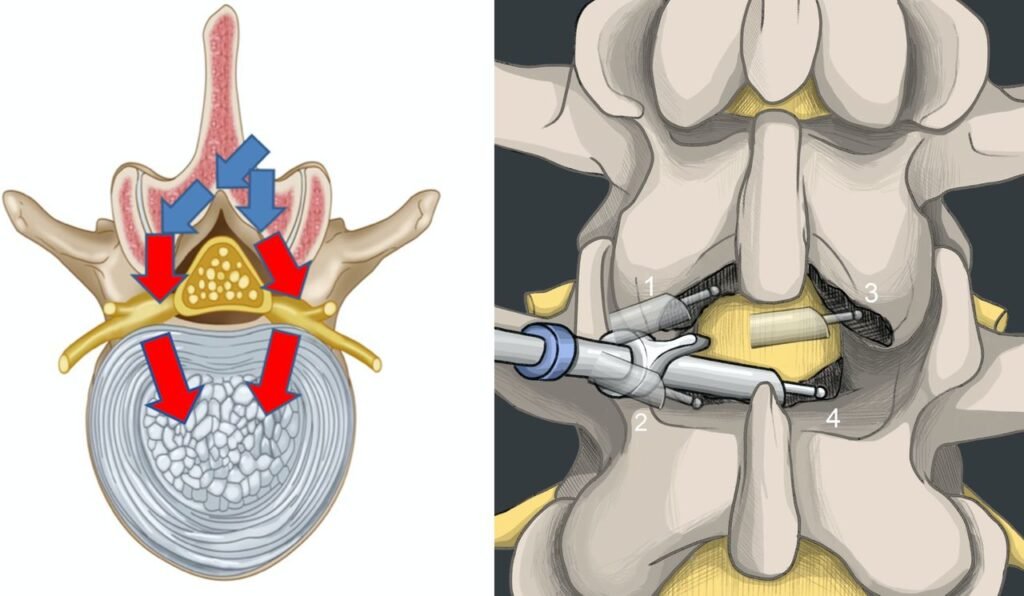
- Surgical Procedure:
- A small incision (5–10 mm) is made over the interlaminar window.
- A guidewire and dilators create a pathway, followed by insertion of the endoscope.
- The endoscope’s camera provides real-time visualization on a monitor.
- Specialized tools (e.g., graspers, lasers, or radiofrequency probes) remove disc material, bone, abscesses, or infected tissue.
- Spinal TB Example: Debridement of a paraspinal abscess or removal of necrotic bone, followed by irrigation to reduce bacterial load.
- The procedure typically lasts 30–90 minutes, depending on complexity.
- Closure and Recovery:
- The incision is closed with sutures or adhesive strips, often requiring minimal stitching.
- Patients are monitored for a few hours and may be discharged the same day (outpatient) or after a short hospital stay (1–2 days).
- Postoperative pain is managed with analgesics, and activity restrictions (e.g., avoiding heavy lifting) are advised for 1–2 weeks.