Minimal Invasive Surgical (MIS) TLIF
- Home >>
- Minimal Invasive Surgical (MIS) TLIF
What is Minimally Invasive Surgical (MIS) TLIF?
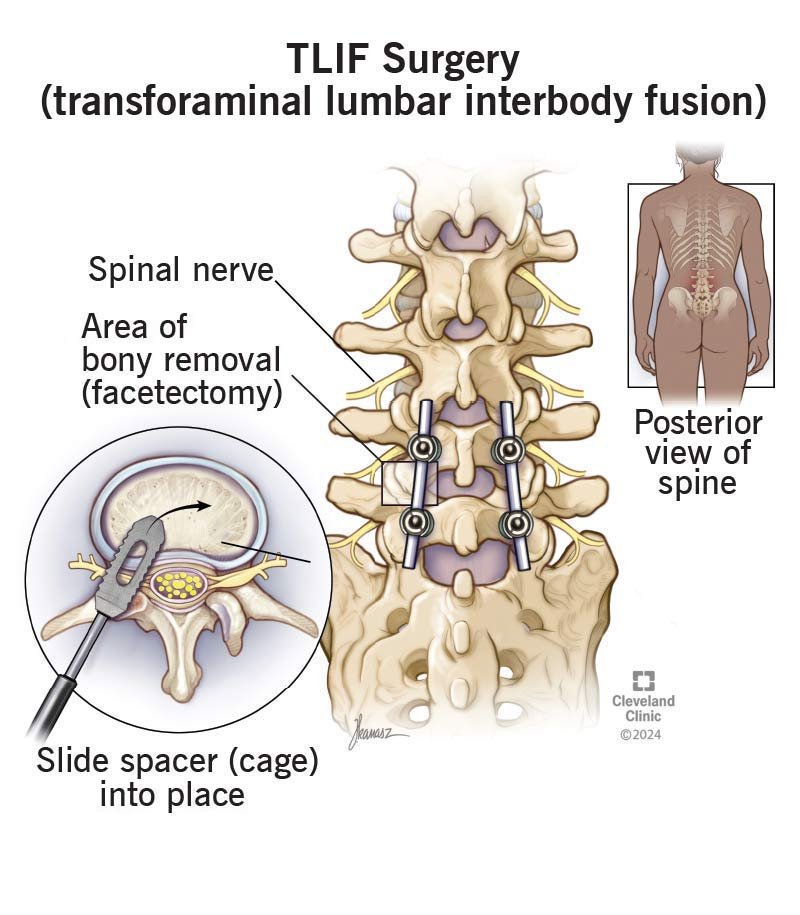
Definition: A minimally invasive procedure to fuse lumbar vertebrae by accessing the disc space through the transforaminal route, placing an interbody cage and bone graft to promote fusion.
Purpose: Stabilizes the spine in conditions like spondylolisthesis, degenerative disc disease, or spinal TB-related instability (e.g., vertebral collapse or kyphosis).
Approach: Uses small incisions, tubular retractors, and fluoroscopy to minimize muscle disruption compared to open TLIF.
Spinal TB Relevance: Addresses TB-related spinal instability or deformity while preserving surrounding tissues, complementing anti-TB therapy.
Context: Likely performed by spine specialists at advanced centers like Sushrut Spine Center for complex lumbar pathologies.
Types of MIS TLIF
Unilateral MIS TLIF: Accesses the disc space from one side, ideal for focal pathology (e.g., TB-related disc destruction).
Bilateral MIS TLIF: Involves both sides for broader decompression and fusion, used in severe instability or multilevel disease.
Percutaneous MIS TLIF: Uses percutaneous screws and rods for fixation, minimizing soft tissue damage, suitable for TB-related cases with minimal deformity.
Endoscopic-Assisted MIS TLIF: Incorporates endoscopic visualization for enhanced precision, applicable for localized TB lesions.
Revision MIS TLIF: Performed to correct failed prior fusions or address recurrent pathology, potentially relevant for chronic TB complications.
Benefits of MIS TLIF
Reduced Tissue Trauma: Smaller incisions (2–3 cm) and less muscle dissection lower postoperative pain and scarring compared to open TLIF.
Faster Recovery: Patients often resume activities within weeks, critical for spinal TB patients needing physiotherapy.
Lower Blood Loss: Minimally invasive tools reduce bleeding, beneficial for TB patients with systemic symptoms like anemia.
Decreased Infection Risk: Smaller wounds and shorter hospital stays (1–2 days) reduce postoperative infections, crucial for immunocompromised TB patients.
Effective Stabilization: Restores spinal alignment and stability, addressing TB-related kyphosis or vertebral collapse while preserving mobility.
Procedure for MIS TLIF
Preoperative Evaluation: MRI/CT confirms pathology (e.g., TB-related instability or disc damage); neurological exams assess deficits; anti-TB therapy may be ongoing.
Surgical Process: Under general anesthesia, small incisions are made; tubular retractors and fluoroscopy guide access to the foramen; disc material is removed, and a cage with bone graft is inserted.
Fixation: Percutaneous pedicle screws and rods stabilize the vertebrae; the procedure lasts 2–4 hours, depending on complexity.
Postoperative Care: Hospital stay of 1–3 days; pain management and early mobilization follow; anti-TB therapy continues for 6–18 months.
Follow-Up: Regular imaging and clinical assessments monitor fusion, neurological recovery, and TB resolution; activity restrictions apply for 6–12 weeks.