Endoscopic minimal Invasive Spine Surgery(Facts & Fiction)
- Home >>
- Endoscopic minimal Invasive Spine Surgery(Facts & Fiction)
Endoscopic Minimally Invasive Spine Surgery: Facts & Fiction
Spine surgery is increasingly leaning toward minimally invasive techniques. Minimally Invasive Spine Surgery (MIS) involves treating spinal conditions through small incisions, minimizing disruption to surrounding muscle tissue.
Benefits of Minimally Invasive Spine Surgery
Small incisions with minimal scar tissue formation
Reduced damage to surrounding muscles and soft tissues
Lower blood loss
Less pain and reduced reliance on pain medication
Faster recovery and quicker return to daily activities
Shorter hospital stays
Many procedures performed as outpatient surgeries
Lower risk of postoperative infections
Open Surgery vs. Minimally Invasive Surgery
Spinal surgeries are classified as either “open” or minimally invasive. An open procedure requires a larger incision, with tissues retracted to allow direct visualization using the naked eye, loupes, or a microscope. Traditionally, this method involves more muscle disruption compared to MIS.
Minimally invasive techniques use specialized tools to operate through smaller incisions with less tissue disturbance, including:
Endoscopic spine surgery
Tubular-assisted microscopic surgery
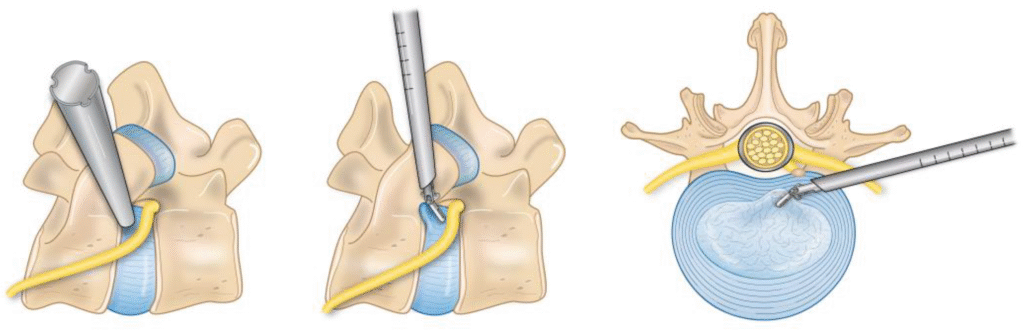
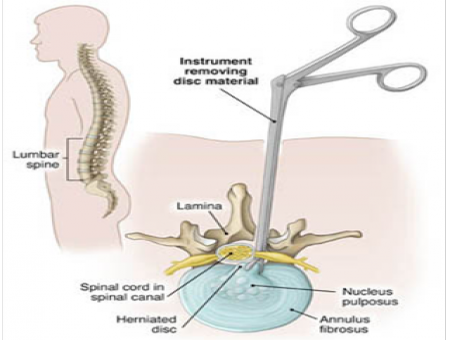
A key tool, the tubular retractor, consists of expanding tubes that gently separate muscles and tissues to access the surgical site, allowing procedures through a narrow channel.
Endoscopic and Endoscopically-Assisted Spine Surgery
An endoscope, a thin fiber-optic camera, provides magnified views of internal structures on a monitor. Surgery is performed by inserting instruments through the endoscope to remove disc material or bone spurs, using a small “keyhole” incision (5-7mm) for true endoscopic surgery. Larger incisions (14-18mm) are used for endoscopically-assisted surgery with a tubular retractor, enhancing visualization.
Laser Spine Surgery
Lasers emit light energy to ablate tissue by converting it to heat. Despite its popularity in marketing, laser spine surgery isn’t a cure-all. The spine’s complexity—bones, discs, joints, nerves, and muscles—makes pinpointing pain sources challenging, and lasers have limitations.
Laser Spine Surgery Myths and Facts
Myth: Laser spine surgery eliminates the need for incisions.
Fact: Lasers require an incision (3mm to over 3 inches) for access, whether through endoscopic, tubular, or open methods.
Myth: Laser surgery can cure spinal arthritis and remove bone spurs causing stenosis.
Fact: Arthritis and bone spurs can’t be “lasered away.” Lasers can’t cut bone; drills and cutting tools are needed to relieve nerve pressure from stenosis. Lasers may ablate facet joint nerves to reduce arthritis pain, similar to radiofrequency ablation.
Myth: Laser surgery is always superior to non-laser surgery.
Fact: While minimally invasive, lasers aren’t suitable for all conditions. Other tools often remove disc material more efficiently through similar small incisions.
Success isn’t guaranteed, and risks remain. Be wary of overly optimistic claims, as some laser centers have faced scrutiny over outcomes.
Summary
Minimally invasive surgery offers a promising alternative for spinal disorders, with faster recovery but a learning curve for surgeons. Results may vary with less experienced practitioners, and not all patients qualify. At Sushrut Spine Center, we’re committed to advancing safe techniques. Contact us for a second opinion to determine if MIS is right for you.